At a glance
Clinicians may have questions about evaluating patients with per- and polyfluoroalkyl substances (PFAS) concerns. Clinicians caring for these patients can review PFAS resources from ATSDR and local or state health department information about PFAS.

What can clinicians do for patients with PFAS exposure concerns?
- Listen carefully to patient health concerns and review them in the context of ATSDR's PFAS information for clinicians and especially information around health risks.
- Help patients identify and reduce major PFAS exposures, such as contaminated drinking water.
- Connect patients to resources, including information from public health agencies, environmental agencies, or occupational and environmental medicine clinicians.
- As some health risks associated with PFAS include outcomes that have recommendations for preventive care, review the patient's medical history and ensure that standard preventive care measures are up to date.
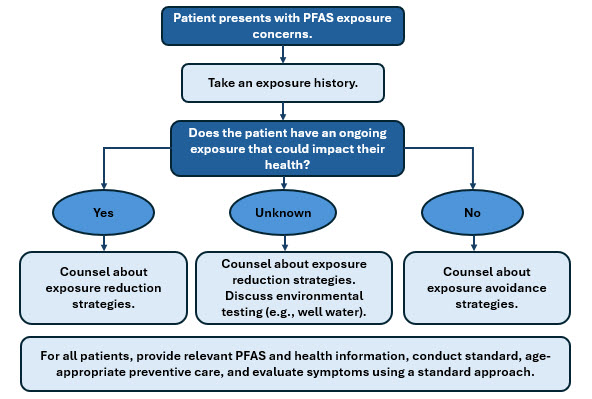
How can clinicians evaluate a patient's PFAS exposure concerns?
- Take an exposure history that includes questions about environmental and occupational exposures. To inform the exposure history, clinicians can:
- Check if local or state public health or environmental agencies have information about PFAS exposures.
- Obtain the results of environmental PFAS testing (e.g., drinking water tests), if available.
- Review ATSDR PFAS Information for Clinicians and Taking an Exposure History Case Study.
- Determine if the patient has an ongoing exposure that could impact their health. (ATSDR's Toxicological Profile for Perfluoroalkyls contains information about assessing exposures for health risks.)
- If yes: Counsel the patient on strategies to reduce exposures. Clinicians can use the patient's exposure history and information from local or state agencies to help identify strategies.
- If unknown: Counsel the patient on strategies to reduce exposures. Help connect the patient with the area's public health or environmental agency to learn about local PFAS contamination issues and whether environmental testing (e.g., private well water testing) is recommended.
- If no: Provide counseling about exposure avoidance strategies.
- Provide relevant PFAS and health information, conduct standard, age-appropriate preventive care, and evaluate symptoms using a standard approach.
Addressing Patient Concerns about PFAS Exposure
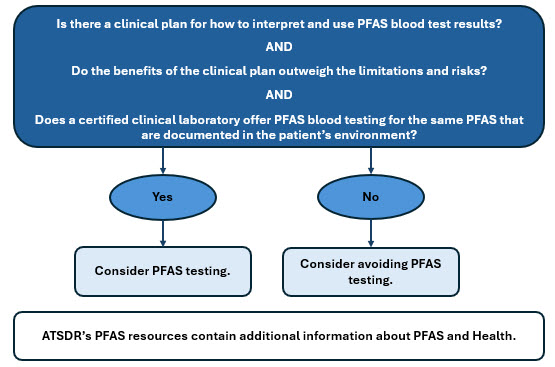
Could a blood test for PFAS help patients with PFAS exposure concerns?
Under certain circumstances, test results may benefit some individuals. Testing can be avoided in other circumstances. When deciding if PFAS blood testing could provide a benefit to a patient's health, clinicians can discuss with the patient:
- How test results will be interpreted and used
- Benefits and limitations of testing (see Box 1 below)
- How PFAS test results can inform clinical decisions and related risks and benefits (ATSDR PFAS Information for Clinicians)
- If a certified clinical laboratory can test the patient's blood for the same PFAS that are documented in the patient's environment, for example in water samples
Assessing Appropriateness of PFAS Blood Testing
What can clinicians do when a patient comes in with a PFAS blood test result?
- Ask why the patient was tested.
- Testing may have occurred as part of a study, due to employment-related exposures, or for another reason.
- Patients may have been motivated by a desire to know if they have been exposed, a belief that their test results may predict their likelihood of getting a disease, or an interest in having additional medical testing done to screen for a PFAS-associated health effect.
- Discuss how testing's benefits and limitations relate to the reason that the patient was tested.
- Take an exposure history and identify strategies to reduce exposures (see ATSDR PFAS Information for Clinicians).
What can I do if a patient has concerns about PFAS exposure and specific symptoms?
PFAS toxicity is not associated with characteristic signs or symptoms. ATSDR encourages clinicians to follow usual standards of care for health concerns.
Is additional medical testing based on specific PFAS blood levels beneficial?
PFAS blood levels do not predict future health outcomes. ATSDR has not identified specific blood levels of PFAS that can be used to determine if additional health screening should be done.
How are patients exposed to PFAS aside from drinking water? If PFAS are everywhere, how can I focus on exposures that matter?
Routes of PFAS exposure differ, even within local communities. Given how common PFAS are in the environment, eliminating all exposures to PFAS may not be possible. By taking an exposure history and understanding the larger exposures occurring in local workplaces or communities, clinicians can help counsel patients on strategies to reduce the most impactful exposures. State and local public health or environmental agencies may have information about local PFAS exposure sources and ways to reduce exposure. Clinicians can reinforce these agencies' messages.
How long will PFAS stay in my patient’s body?
The half-lives of PFAS vary by specific PFAS and patient-specific factors (e.g., kidney function). Some PFAS have half-lives of years. ATSDR's Toxicological Profile for Perfluoroalkyls provides a detailed review.
Can a fetus be exposed to PFAS?
Some PFAS cross the placenta and enter umbilical cord blood. The permeability of the placental barrier varies for different PFAS.
Is there a specific treatment for PFAS exposure?
No approved medical treatments are available to reduce PFAS in the body; however, there is ongoing research into therapeutic approaches. Exposure reduction is the primary strategy to help patients with PFAS exposures that may pose health risks.
What counseling can clinicians provide patients about exposure reduction?
- When possible, choose products without PFAS. For examples of products that can contain PFAS see ATSDR's PFAS Information for Clinicians section on Human Exposure to PFAS.
- Limit or avoid fish, meat, eggs, or dairy known to be contaminated with PFAS. Use local health advisories and EPA's fish advisory list to guide choices.
- Clean surfaces and floors frequently if soil around the home is contaminated or if household members have occupational exposure to PFAS.
- Handwashing may reduce the chance of ingesting PFAS-containing dust.
- Test private well water. Consult local health or environmental agencies for guidance on private well testing.
Should a nursing mother continue to breastfeed?
Due to the many benefits of breastfeeding, the Centers for Disease Control and Prevention (CDC) and American Academy of Pediatrics recommend that most nursing women continue to breastfeed.
Is it beneficial to retest patients if they have a detectable PFAS level? If so, when?
Clinicians can discuss with patients the benefits and limitations of retesting, including how the test will inform clinical care. Neither the utility of repeat PFAS blood testing nor the optimum interval for retesting is known.
Will insurance cover PFAS visits and tests? What billing codes could I use?
Insurance coverage varies. Clinicians and patients can confirm coverage with the patient's insurer. Codes for PFAS-related clinical encounters and PFAS blood testing have not been standardized. However, there are ICD-10-CM (the International Classification of Diseases, Tenth Revision, Clinical Modification) codes related to contact with environmental pollution. Clinical laboratories may provide suggested Current Procedural Terminology (CPT®) codes.
For more information, visit atsdr.cdc.gov/pfas

