Who Is at Risk of Lead Exposure?
“In the late 1700s, Ben Franklin described various environmental and occupational effects which he attributed to lead, affecting trades, such as printers, plumbers, and painters. In the early 1900s, detailed information on the hazards began to appear. First, a study in Britain linked exposures to lead with high rates of infertility, stillbirths, and first year infant deaths. About the same time, an Australian study observed lead poisoning among children and identified household dust and paint as the sources of the lead. Childhood activities, such as nail-biting, thumb-sucking, and eating with fingers contaminated with lead are the ways lead was introduced into the body” [DOT 2016b].
Both children and adults are susceptible to health effects from lead exposure, although the typical exposure pathways and effects can be somewhat different.
- Children who reside in pre-1978 housing (and especially those in inner cities, where a large number of older rental homes exist, or homes built before 1950) are at greatest risk for exposure, because older housing may contain paint with higher lead content.
- “Childhood lead exposure has a significant and persistent impact on brain reorganization associated with language function” [Yuan et al. 2006].
- Adults who work in jobs involving lead are occupationally exposed.
- Developing fetuses are also at risk for adverse health outcomes (less than 1% of the mothers have levels greater than or equal to 5 micrograms per deciliter, or μg/dL), as levels that present risk to the fetus may not present risk to the mother.
- Smokers and their relatives (if exposed to secondhand smoke) are at a high risk for exposure due to the lead in tobacco smoke.
While children’s blood lead levels (BLLs) have steadily declined in recent decades, there are still an estimated 535,000 U.S. children ages 1-5 years with BLLs at or above the upper reference source range value of 5 µg/dL [CDC 2013g]. This was calculated using the 20072010 National Health and Nutrition Examination Survey [NHANES] cycle that showed 2.6% of children in this age group, with levels above 5 mcg/dL, based on the U.S. Census Bureau 2010 count [CDC 2013g].
- In particular, children who live in older housing are more likely to have elevated BLLs than U.S. children as a whole.
- No economic or racial/ethnic subgroup of children is free from the risk of adverse health effects due to high BLLs.
- Of the 434,000 children reported with confirmed elevated BLLs (≥10 µg/dL) between 1997 and 2001 (2.2% of children aged 1-5 years), approximately
- 17% were non-Hispanic whites,
- 60% were non-Hispanic African-Americans,
- 16% were Hispanic, and
- 7% were of other races or ethnicities [CDC 2003].
- The children affected are more likely to be poor and from racial/ethnic minority groups living in substandard housing. African-American children remain at increased risk for higher blood lead concentration after adjusting for environmental lead exposures and dietary intake [Lanphear et al. 2002].
Because of their behavior and physiology, children are more affected by exposure to lead than adults.
- Children absorb more ingested lead than do adults.
- Children generally ingest lead-contaminated soil and house dust at higher rates than adults because of mouthing and hand-to-mouth behaviors.
- Children who exhibit pica, a compulsive hand-to-mouth behavior and repeated eating of non-food items -not considered pathologic in infants and toddlers up to 2 years of age-, are at greatest risk.
- Children have a higher breathing rate than adults, breathing in a greater volume of air per pound.
- Being shorter than adults, children are more likely to breathe lead-contaminated dust and soil as well as lead-containing fumes close to the ground.
- The percent of lead absorbed in the gut, especially in an empty stomach, is estimated to be as much as 5 to 10 times greater in infants and young children than in adults [Ziegler et al. 1978 as cited in ATSDR 1999; James et al. 1985; Chamberlain et al. 1978; Alexander et al. 1974].
- Gastrointestinal absorption of lead in children is increased by deficiencies in
- Ascorbate,
- Calcium,
- Iron, and
- Zinc [Mahaffey 1990, as cited in AAP 1993].
Lead in dust and water can contribute up to 35% and 20% respectively to lead exposure in children’s Blood Lead Levels (Figure 1).
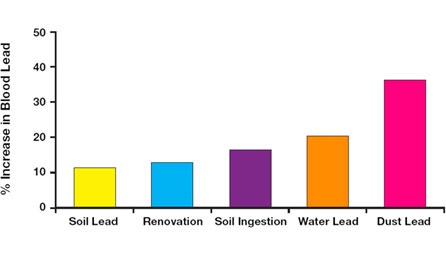
Figure 1. Sources of Contribution of Lead Exposure to Children’s Blood Lead Concentrations [AAP 2016, adapted from Lanphear et al. 2012, and Spanier et al. 2013]
Children are more sensitive than adults to elevated BLLs. Children’s developing brains, nervous system, and other organ systems are very sensitive to lead. Differences between the adult blood brain barrier and that of fetuses and very young children, increases the risk of lead’s entry into the developing central nervous system of the latter two. This can result in prolonged or permanent neurobehavioral disorders.
- Childhood lead exposure is inversely associated with
- Brain reorganization associated with language function [Yuan et al. 2006],
- Intellectual abilities [Lanphear et al. 2005],
- Academic achievement,
- Psychomotor development [Lanphear et al. 2005],
- High school attendance,
- Reaction times,
- Class rank,
- Hand and-eye coordination, and
- Vocabulary and grammatical reasoning scores [AAP 1993].
- “Blood lead concentrations <5 µg/dL are associated with intellectual deficits (lower IQ score), academic disabilities, attention-related behaviors, and problem behaviors” [Landrigan and Etzel 2014].
- Lanphear et al. [2005] report a deficit of approximately 2 IQ points for the Blood Lead variable of 10-20 µg/dL. The decrements in IQ associated with lead were found to be proportionately greater at the lowest blood lead levels [Landrigan and Etzel 2014; Bellinger 2008]. “At lower concentrations of lead in the blood – below 10 µg/dL -children tested for IQ at ages three and five, showed a greater decline in IQ for a rise in blood lead from 1 to 10 µg/dL, than those whose blood lead level went from 10 to 20 µg/dL” [Canfield et al. 2003].
- “The blood lead concentration was inversely and significantly associated with IQ. In the linear model, each increase of 10 µg per deciliter in the lifetime average blood lead concentration was associated with a 4.6-point decrease in IQ (P=0.004), whereas for the subsample of 101 children whose maximal lead concentrations remained below 10 µg per deciliter, the change in IQ associated with a given change in lead concentration was greater. When estimated in a nonlinear model with the full sample, IQ declined by 7.4 points as lifetime average blood lead concentrations increased from 1 to 10 µg per deciliter” [Canfield et al. 2003].
- “Early childhood lead exposure is associated with poorer achievement on standardized reading and math tests in the third grade, even at very low B-Pbs” [Evens et al. 2015].
- “Children with moderate lead poisoning in early childhood performed significantly lower on all components of elementary school end-of-grade examinations compared with unexposed children” [Magzamen et al. 2013].
- Even low-level lead exposure can negatively impact a wide range of cognitive functions, such as attention, language, memory, cognitive flexibility, and visual-motor integration based on various types of neuropsychological and neurobehavioral testing [Canfield et al. 2004; Canfield et al. 2003].
- “For every 1 µg/dL increase in blood lead concentration, there was a 0.7-point decrement in mean arithmetic scores, an approximately 1-point decrement in mean reading scores, a 0.1-point decrement in mean scores on a measure of nonverbal reasoning, and a 0.5-point decrement in mean scores on a measure of short-term memory. An inverse relationship between blood lead concentration and arithmetic and reading scores was observed for children with blood lead concentrations lower than 5.0 µg/dL” [Lanphear et al. 2000].
- Children’s renal, endocrine, and hematological systems may also be adversely affected by lead exposure.
Children are also exposed to lead through second-hand tobacco smoke [Apostolou et al. 2012; Mannino et al. 2005; Mannino et al. 2003].
There is no known threshold exposure level (as indicated by BLL) for many of these effects. No blood lead threshold for adverse health effects has been identified in children, however, more severe effects occur at higher levels and more subtle effects, some not clinically recognizable, at very low levels.
Preventing lead exposure in early childhood is critical to improving school performance [Evens et al. 2015; Lanphear et al. 2005].
“The consequences of exposure to many other chemicals or mixtures of chemicals, such as insecticides -chemicals oftentimes specifically designed to be toxic- are largely unknown. Many of these chemicals or their metabolites are routinely found in the blood and body fluids of pregnant women and children” [Lanphear et al. 2005].
Although children are at greater risk from lead exposure, adult exposures can also result in harmful health effects.
- Most adult exposures are occupational and occur in lead-related industries such as [CDC 2016]
- Manufacturing,
- Construction,
- Services, and
- Mining.
- One frequent source of lead exposure to adults is home renovation that involves
- Scraping,
- Remodeling, or
- Otherwise disturbing lead-based paint.
Renovation involving lead based paint should only be undertaken after proper training, or with the use of certified personnel (see EPA’s Safe Renovation brochure at http://www2.epa.gov/lead/lead-safecertified-guide-renovate-right.
Adults can also be exposed during certain hobbies and activities where lead is used [CDC 2011a]. Some of the more common examples include
- Artistic painting,
- Car repair,
- Electronics soldering,
- Glazed pottery making,
- Metal soldering,
- Molding of bullets, slugs, or fishing sinkers,
- Stained-glass making, and
- Shooting firearms.
Tobacco smoke is a source of lead [Apostolou et al. 2012; Mannino et al. 2005; Mannino et al. 2003].
Mine workers may inhale lead dust and lead oxide fumes if they
- Eat,
- Drink, and
- Smoke in or near contaminated areas, thereby increasing their probability of lead ingestion.
If showers and changes of clothing are not provided, workers can contaminate their homes and/or vehicles with lead dust on their
- Hair,
- Skin,
- Shoes,
- Clothing, and
- Tools
thus inadvertently exposing family members.
People who use the following items also increase their lead exposure risk:
- Paints, pigments,
- Facial makeup, or
- Hair coloring with lead or lead acetate.
Cosmetics containing lead include
- Surma,
- Sindhoor and
- Kohl, popular in certain Asian countries.
Other than the developmental effects unique to young children, the health effects experienced by adults from adult exposures are similar to those experienced by children, although the thresholds are generally higher.
Table 2. Populations at Risk of Exposure to Lead in the Workplace
Auto repairers
Auto repairers
Lead refining workers
Lead refining workers
Battery manufacturers and recycling
Battery manufacturers and recycling
Lead smelter workers
Lead smelter workers
Bridge reconstruction workers
Bridge reconstruction workers
Plastic manufacturers
Plastic manufacturers
Construction workers
Construction workers
Plumbers, pipe fitters
Plumbers, pipe fitters
Firing range instructors
Firing range instructors
Police officers
Police officers
Glass manufacturers
Glass manufacturers
Printers
Printers
Lead manufacturers industry employees
Lead manufacturers industry employees
Rubber product manufacturing
Rubber product manufacturing
Lead mining workers
Lead mining workers
Shipbuilders
Shipbuilders
Workers in recycling plants for electronics, computers, etc
Workers in recycling plants for electronics, computers, etc
Steel welders or cutters
Steel welders or cutters
The mother’s BLL is an important indication of risk to the fetus and neurological problems in newborns. In addition, mothers who had exposure to lead in the past may store lead in their bones. Lead may be released from bones during times of calcium stress such as pregnancy and lactation. Pregnant women with elevated BLLs may have an increased chance of
- Preterm labor,
- Miscarriage,
- Neurological effects and intrauterine growth restriction (IUGR),
- Spontaneous abortion or stillbirth, and/or
- Low birth weight.
See the “What are Possible Health Effects from Lead Exposure?” section for more information.
Table 3. Risk Factors for Lead Exposure in Pregnant and Lactating Women [CDC 2012]
Recent immigration from or residency in areas where ambient lead contamination is high, e.g., from countries where leaded gasoline is still being used (or was recently phased out), or where industrial emissions are not well-controlled.
Recent immigration from or residency in areas where ambient lead contamination is high, e.g., from countries where leaded gasoline is still being used (or was recently phased out), or where industrial emissions are not well-controlled.
Living near a source of lead, such as lead mines, smelters, or battery recycling plants (even if the establishment is closed).
Living near a source of lead, such as lead mines, smelters, or battery recycling plants (even if the establishment is closed).
Working with lead or living with someone who does (take-home exposures).
Working with lead or living with someone who does (take-home exposures).
Cooking, storing, or serving food in lead-glazed ceramic pottery made in a traditional process and usually imported by individuals outside the normal regulatory commercial channels.
Cooking, storing, or serving food in lead-glazed ceramic pottery made in a traditional process and usually imported by individuals outside the normal regulatory commercial channels.
Eating or mouthing non-food items (pica) that may be contaminated with lead (such as soil, clay, or lead-glazed ceramic pottery).
Eating or mouthing non-food items (pica) that may be contaminated with lead (such as soil, clay, or lead-glazed ceramic pottery).
Using alternative or complementary medicines, herbs, or therapies for home remedies or certain traditional herbs that may be contaminated with lead.
Using alternative or complementary medicines, herbs, or therapies for home remedies or certain traditional herbs that may be contaminated with lead.
Using imported cosmetics, such as kohl or surma, or certain imported foods or spices that may be contaminated with lead.
Using imported cosmetics, such as kohl or surma, or certain imported foods or spices that may be contaminated with lead.
Engaging in certain high-risk hobbies or recreational activities, like leaded glass, hunting, or jewelry making (if using leaded products), and those who have family members who do.
Engaging in certain high-risk hobbies or recreational activities, like leaded glass, hunting, or jewelry making (if using leaded products), and those who have family members who do.
Renovating or remodeling older homes without using safe lead work practices.
Renovating or remodeling older homes without using safe lead work practices.
Disturbing higher lead content paint and/or creating lead dust, or spending time in such a home environment.
Disturbing higher lead content paint and/or creating lead dust, or spending time in such a home environment.
Consuming lead-contaminated drinking water from homes with leaded pipes or source lines with lead.
Consuming lead-contaminated drinking water from homes with leaded pipes or source lines with lead.
Having a history of previous lead exposure or evidence of elevated body burden of lead from past exposures, particularly with a deficiency in certain key nutrients (e.g., calcium, iron).
Having a history of previous lead exposure or evidence of elevated body burden of lead from past exposures, particularly with a deficiency in certain key nutrients (e.g., calcium, iron).
Living with someone identified with an elevated BLL.
Living with someone identified with an elevated BLL.
Having exposures in common with a child, close friend, or other relative living in the same environment.
Having exposures in common with a child, close friend, or other relative living in the same environment.
- Today, children who live in pre-1978 housing are the population generally at greatest risk for lead poisoning.
- Adults who work with lead or have hobbies involving lead may also be significantly exposed.
- Developing fetuses exposed to lead are also at risk for adverse health outcomes.
- Children may also be exposed to lead through second-hand tobacco smoke.